Baccalaureate and graduate education for professional nursing include processes that foster the development of values, attitudes, personal qualities, and value-based professional behaviors. Values are defined as beliefs or ideals to which the individual is committed and which guide behavior. Values are reflected in attitudes, personal qualities, and consistent patterns of behavior. Attitudes are inclinations or dispositions used to respond to persons or situations, while personal qualities are innate or learned attributes of an individual. Professional behaviors reflect the individual’s commitment to specific professional values.
The professional nurse must adopt characteristics such as independence, assertiveness, self-esteem, and confidence, as well as demonstrating compassion, acceptance, consideration, and kindness. Adoption of essential values leads the nurse to a sense of commitment and social responsibility, sensitivity and responsiveness to the needs of others, and a responsibility for oneself and one’s actions (AACN, 2008).
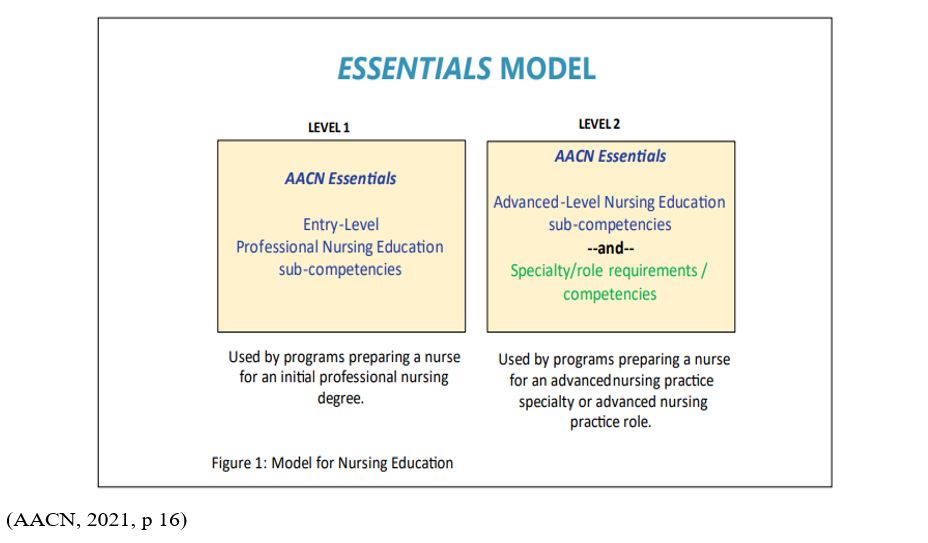
The School of Nursing values are adapted The Essentials: Core Competencies for Professional Nursing Education Domains and Concepts of Competent Practice (AACN, 2021, pp 9-14):
- Domain 1: Knowledge for Nursing Practice
Descriptor: Integration, translation, and application of established and evolving disciplinary nursing knowledge and ways of knowing, as well as knowledge from other disciplines, including a foundation in liberal arts and natural and social sciences. This distinguishes the practice of professional nursing and forms the basis for clinical judgment and innovation in nursing practice. - Domain 2: Person-Centered Care
Descriptor: Person-centered care focuses on the individual within multiple complicated contexts, including family and/or important others. Person-centered care is holistic, individualized, just, respectful, compassionate, coordinated, evidence-based, and developmentally appropriate. Person-centered care builds on a scientific body of knowledge that guides nursing practice regardless of specialty or functional area. - Domain 3: Population Health
Descriptor: Population health spans the healthcare delivery continuum from public health prevention to disease management of populations and describes collaborative activities with both traditional and non-traditional partnerships from affected communities, public health, industry, academia, health care, local government entities, and others for the improvement of equitable population health outcomes. - Domain 4: Scholarship for Nursing Practice
Descriptor: The generation, synthesis, translation, application, and dissemination of nursing knowledge to improve health and transform health care. - Domain 5: Quality and Safety
Descriptor: Employment of established and emerging principles of safety and improvement science. Quality and safety, as core values of nursing practice, enhance quality and minimize risk of harm to patients and providers through both system effectiveness and individual performance. - Domain 6: Interprofessional Partnerships
Descriptor: Intentional collaboration across professions and with care team members, patients, families, communities, and other stakeholders to optimize care, enhance the healthcare experience, and strengthen outcomes. - Domain 7: Systems-Based Practice
Descriptor: Responding to and leading within complex systems of health care. Nurses effectively and proactively coordinate resources to provide safe, quality, equitable care to diverse populations. - Domain 8: Information and Healthcare Technologies
Descriptor: Information and communication technologies and informatics processes are used to provide care, gather data, form information to drive decision making, and support professionals as they expand knowledge and wisdom for practice. Informatics processes and technologies are used to manage and improve the delivery of safe, high- quality, and efficient healthcare services in accordance with best practice and professional and regulatory standards. - Domain 9: Professionalism
Descriptor: Formation and cultivation of a sustainable professional nursing identity, accountability, perspective, collaborative disposition, and comportment that reflects nursing’s characteristics and values. - Domain 10: Personal, Professional, and Leadership Development
Descriptor: Participation in activities and self-reflection that foster personal health, resilience, and well-being, lifelong learning, and support the acquisition of nursing expertise and assertion of leadership.
Concepts of Competent Practice
- Clinical Judgment
As one of the key attributes of professional nursing, clinical judgment refers to the process by which nurses make decisions based on nursing knowledge (evidence, theories, ways/patterns of knowing), other disciplinary knowledge, critical thinking, and clinical reasoning (Manetti, 2019). This process is used to understand and interpret information in the delivery of care. Clinical decision making based on clinical judgment, is directly related to care outcomes. - Communication
Communication, informed by nursing and other theories, is a central component in all areas of nursing practice. Communication is defined as an exchange of information, thoughts, and feelings through a variety of mechanisms. The definition encompasses the various ways people interact with each other, including verbal, written, behavioral, body language, touch, and emotion. Communication also includes intentionality, mutuality, partnerships, trust, and presence. Effective communication between nurses and individuals and between nurses and other health professionals is necessary for the delivery of high quality, individualized nursing care. With increasing frequency communication is delivered through technological modalities. Communication also is a core component of team-based, interprofessional care and closely interrelated with the concept Social Determinants of Health (described below). - Compassionate Care
As an essential principle of person-centered care, compassionate care refers to the way nurses relate to others as human beings and involves “noticing another person’s vulnerability, experiencing an emotional reaction to this, and acting in some way with them in a way that is meaningful for people” (Murray & Tuqiri, 2020). Compassionate care is interrelated with other concepts such as caring, empathy, and respect and is also closely associated with patient satisfaction. - Diversity, Equity, and Inclusion
Collectively, diversity, equity, and inclusion (DEI) refers to a broad range of individual, population, and social constructs and is adapted in the Essentials as one of the most visible concepts. Although these are collectively considered a concept, differentiation of each conceptual element leads to enhanced understanding.
Diversity references a broad range of individual, population, and social characteristics, including but not limited to age; sex; race; ethnicity; sexual orientation; gender identity; family structures; geographic locations; national origin; immigrants and refugees; language; any impairment that substantially limits a major life activity; religious beliefs; and socioeconomic status. Inclusion represents environmental and organizational cultures in which faculty, students, staff, and administrators with diverse characteristics thrive. Inclusive environments require intentionality and embrace differences, not merely tolerate them (AACN, 2017; Bloomberg, 2019). Everyone works to ensure the perspectives and experiences of others are invited, welcomed, acknowledged, and respected in inclusive environments. Equity is the ability to recognize the differences in the resources or knowledge needed to allow individuals to fully participate in society, including access to higher education, with the goal of overcoming obstacles to ensure fairness (Kranich, 2001). To have equitable systems, all people should be treated fairly, unhampered by artificial barriers, stereotypes, or prejudices (Cooper, 2016). Two related concepts that fit within DEI include structural racism and social justice (See the glossary for definitions structural racism and social justice). - Ethics
Core to professional nursing practice, ethics refers to principles that guide a person’s behavior. Ethics is closely tied to moral philosophy involving the study of or examination of morality through a variety of different approaches (Tubbs, 2009). There are commonly accepted principles in bioethics that include autonomy, beneficence, non-maleficence, and justice (ANA 2015; ACNM, 2015; AANA, 2018; ICN, 2012). The study of ethics as it relates to nursing practice has led to the exploration of other relevant concepts, including moral distress, moral hazard, moral community, and moral or critical resilience. - Evidence-Based Practice
The delivery of optimal health care requires the integration of current evidence and clinical expertise with individual and family preferences. Evidence-based practice is a problem- solving approach to the delivery of health care that integrates best evidence from studies and patient care data with clinician expertise and patient preferences and values (Melnyk, Fineout-Overhold, Stillwell, & Williamson, 2010). In addition there is a need to consider those scientific studies that ask: whose perspectives are solicited, who creates the evidence, how is that evidence created, what questions remain unanswered, and what harm may be created? Answers to these questions are paramount to incorporating meaningful, culturally safe, evidence-based practice (Nursing Mutual Aid, 2020). - Health Policy
Health policy involves goal directed decision-making about health that is the result of an authorized public decision-making process (Keller & Ridenour, 2021). Nurses play critical roles in advocating for policy that impacts patients and the profession, especially when speaking with a united voice on issues that affect nursing practice and health outcomes. Nurses can have a profound influence on health policy by becoming engaged in the policy process on many levels, which includes interpreting, evaluating, and leading policy change. - Social Determinants of Health
Determinants of health, a broader term, include personal, social, economic, and environmental factors that impact health. Social determinants of health, a primary component of determinants of health “are the conditions in the environment where people are born, live, learn, work, play, worship, and age that affect a wide range of health, functioning, and quality of life outcomes and risks.”
The social determinants of health contribute to wide health disparities and inequities in areas such as economic stability, education quality and access, healthcare quality and access, neighborhood and built environment, and social and community context (Healthy People, 2030). Nursing practices such as assessment, health promotion, access to care, and patient teaching support improvements in health outcomes. The social determinants of health are closely interrelated with the concepts of diversity, equity, and inclusion, health policy, and communication.